Why Personalization Matters
No two fertility journeys are alike. Age, hormone levels, underlying health conditions, and emotional well-being all play a role in conception. That’s why IVF centres today emphasize personalized care, shifting away from standard treatment protocols. Personalization doesn’t just improve your comfort, it increases the likelihood of success. Instead of treating everyone the same, clinics now look at patients holistically, identifying what your body needs most. This approach ensures fewer failed cycles.
Initial Fertility Assessment
Before any treatment plan is created, a detailed assessment of both partners is carried out. This includes hormonal blood tests, ovarian reserve testing, ultrasound scans, semen analysis, and sometimes, advanced diagnostics like hysteroscopy. Understanding what works for you based on your unique profile is the first step in creating an IVF plan that’s realistic and effective. Doctors also use this data to foresee potential obstacles and prepare for them in advance.
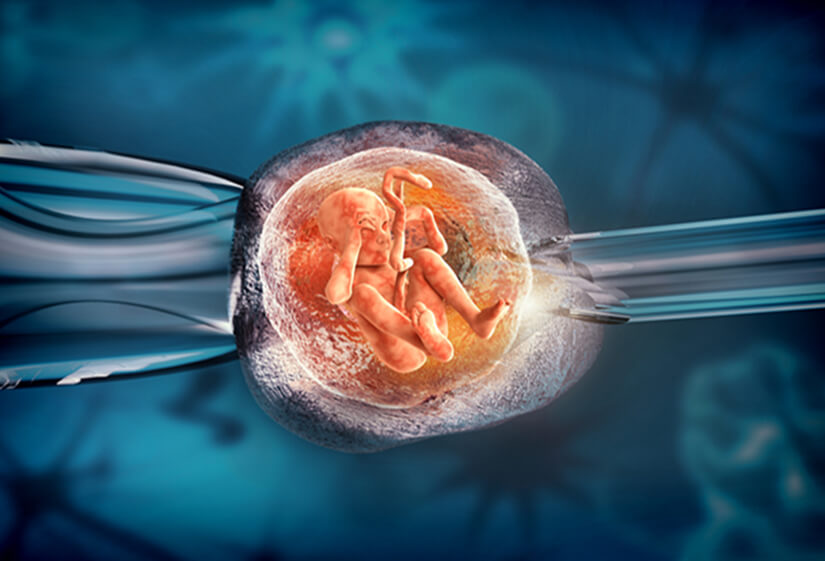
Genetic Testing and Embryo Screening as Decision Tools
Preimplantation Genetic Testing (PGT) is now frequently used to ensure only healthy embryos are transferred, especially for couples with a history of miscarriage or genetic disorders. Genetic screening adds an extra layer of precision to IVF planning. It allows specialists to identify embryos with chromosomal abnormalities that might otherwise lead to failed implantation or pregnancy loss. Not every couple needs PGT, but for many it’s very useful.
Ovarian Stimulation Protocols
Ovarian stimulation is an important step in IVF, and it’s not the same for everyone. Doctors now customize the medication dosage and protocol depending on how a patient’s ovaries respond to hormones. Some may benefit from an aggressive stimulation, while others might need a more gentle approach. Monitoring hormone levels and follicle growth during the cycle allows real-time adjustments. This helps reduce risks like ovarian hyperstimulation syndrome (OHSS).
Male Factor Infertility
Infertility is not just a women’s issue. Nearly half of infertility cases involve male factors. Personalization here means going beyond a basic semen analysis to evaluate DNA fragmentation, motility patterns, or underlying infections. Based on results, treatments like ICSI (Intracytoplasmic Sperm Injection), sperm washing, or testicular sperm retrieval may be considered.
Lifestyle, Stress, and Hormone Mapping in Treatment Planning
Stress, sleep, nutrition, and hormonal imbalances can all affect fertility outcomes. A growing number of IVF centres now integrate lifestyle evaluations and support into treatment planning. From recommending supplements to stress management techniques like acupuncture and yoga, patients are encouraged to improve their overall well-being before and during treatment. This approach ensures that IVF isn’t just about medication and labs but about optimizing the body’s readiness to conceive and carry a pregnancy.
Technology-driven Monitoring and Real-time Cycle Adjustments
Advanced IVF centres now rely on digital hormone tracking, AI-based embryo selection tools, and real-time ultrasound imaging to tweak treatment protocols as needed. For instance, if a patient responds too slowly or quickly to stimulation, medication can be adjusted immediately. These real-time decisions, powered by data, make treatments more responsive and less prone to failure. Technology allows doctors to catch small changes before they become problems in the future.
Bangalore has become a hub for quality fertility care, with its combination of skilled specialists, advanced infrastructure, and a patient-centered mindset. The city is known for integrating modern technology with care, making it ideal for couples seeking a good IVF journey. If you’re looking for care that is personal to you, the best IVF centre in Bangalore will likely offer just that.
Counseling and Emotional Support as Part of Personalized Care
IVF can be emotionally exhausting. The physical strain of hormones and procedures is often matched by anxiety, isolation, and fear of failure. That’s why mental health professionals are now being included into fertility teams. Individual and couple counseling, group therapy, or even simple check-ins help normalize the emotional ups and downs of IVF.